As the operator of five hospitals in the metropolitan area at the time, we at Swedish Health Services found ourselves face-to-face with a public health crisis unlike anything we could have imagined. The highly contagious SARS-CoV-2 virus was fast-moving, unpredictable, and insidious. “Unprecedented” is the word we all used back then; I know we’re all tired of that term today, but honestly, it’s still the best word to describe that singularly chaotic moment. We weren’t just experiencing a once-in-a-hundred-years pandemic; we were at the heart of it.
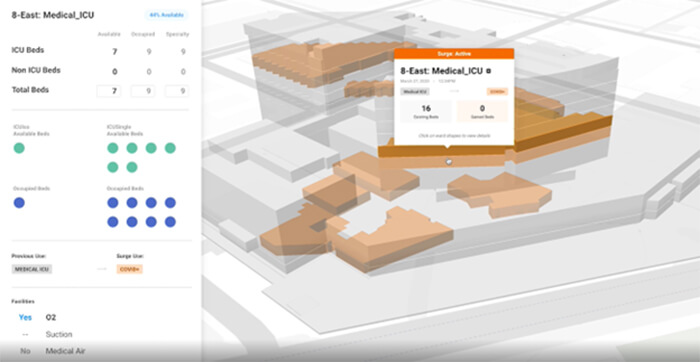
We knew we had to prepare for surges—extraordinarily large numbers of COVID-positive patients in need of medical care all at the same time—so it couldn’t just be business as usual. We had to have a better handle on how many beds were available across our network of hospitals at any given minute (literally, beds were filling up that quickly). We also had to know how many rooms needed to be retrofitted with special medical equipment, like negative-pressure HVAC systems that minimize the risk of airborne viral spread. In those early days, we were printing out floor plans and facility diagrams every morning and pinning them on bulletin boards in our COVID command center. Our administrative staff would then manually mark them up as the day went on to map out patient bed availability. It was a very slow, painstaking process, but it’s what we had to do.