By Sabah Mohammed, E. Todd Wheeler Fellow, Class of 2021
In a resource-rich country like the United States, health care spending in 2020 reached an all-time high of $4.1 trillion, or $12,530 per citizen. That’s twice the GDP (Gross Domestic Product) of India, a populous country with four times the population of the United States. But even so, we rank poorly on every measure of health status.
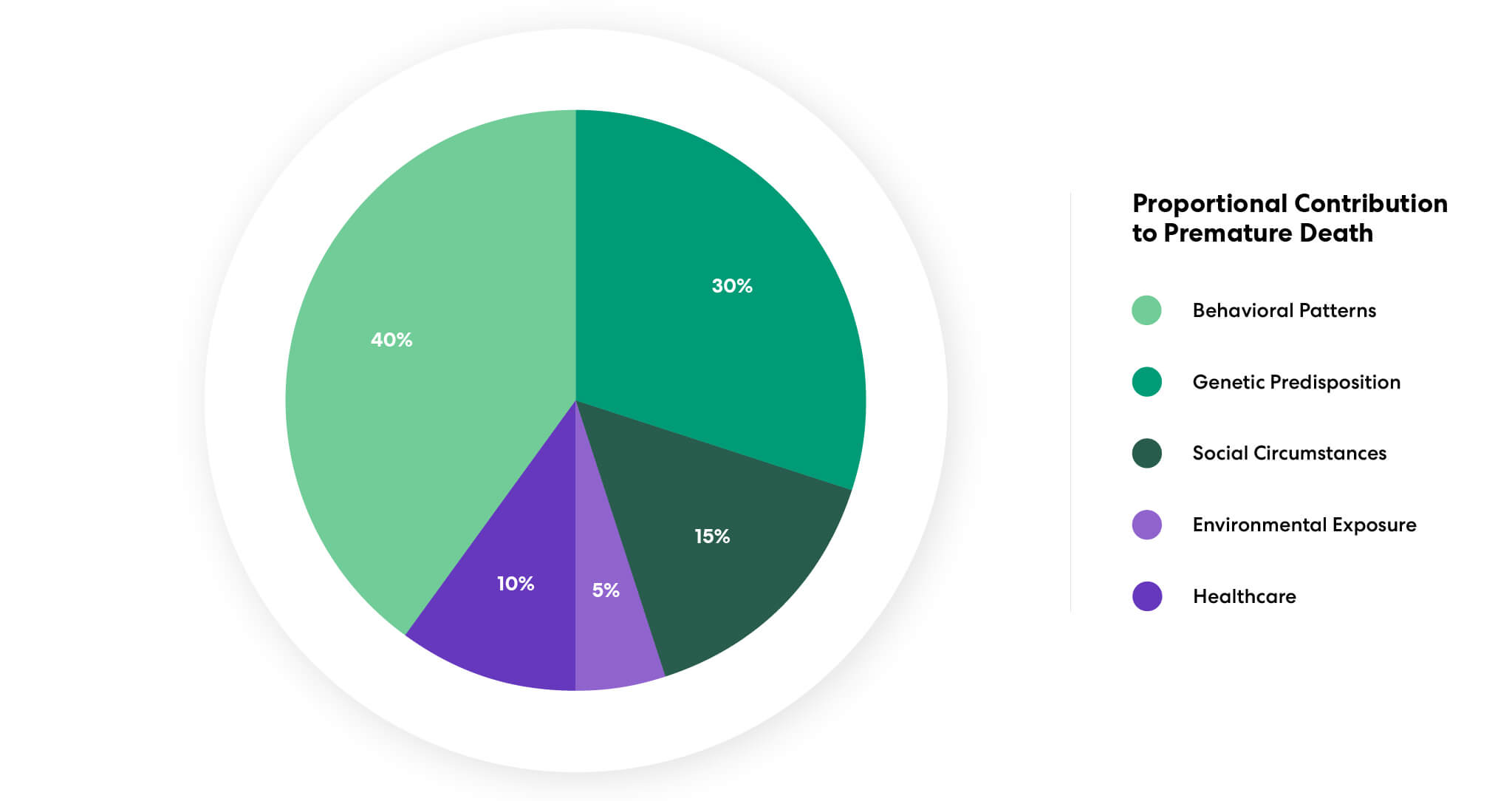
As baffling as this incongruity is, there is a growing consensus that pathways to better health do not necessarily depend entirely on better healthcare. Health is driven by five domains: genetic predisposition, social circumstances, environmental exposure, behavioral patterns, and quality of health care. The built environment directly or indirectly affects environmental exposure and behavioral patterns. Consequently, the built environment is a critical leverage point to drive healthy outcomes for populations that spend more than 90% of their time indoors, if not more during the peak of the COVID-19 pandemic. The built environment and human behavior continue to be shaped by the aftermath of COVID-19, and there is a renewed focus on designing for human health and well-being. As an E. Todd Wheeler Fellow, this National Public Health Week, I reflect on his legacy and pursuit of answers to some of the most pressing challenges in healthcare design.